
By Scott D. Ganz, DMD
Prosthodontics, Maxillofacial
Prosthetics & Implant Dentistry
While CBCT imaging and interactive software provide the foundation for proper diagnosis and treatment planning, ultimately it is the clinician that determines the drilling protocol, and when implants should be loaded. The diagnostic and planning phase can only subjectively estimate whether an implant will be stable within the bone. Resonance Frequency Analysis (RFA) provides a true objective assessment regarding implant stability helping clinicians to determine when implant can be restored.
Therefore, clinicians must use this invaluable tool to assess receptor sites as to implant stability to avoid complications and provide accurate outcomes. RFA/Osstell ISQ imparts this crucial knowledge. Additionally, the non-destructive methodology reveals the status of the integration process at insertion, uncovering, loading, final restoration, and throughout the lifespan of the implant(s).
Maxillary Central Incisor Implant Supported Crown – Brief Case Report
A patient presented with a failing maxillary central incisor tooth post apicoectomy. The CBCT revealed that it would be difficult to gain stability for an immediate implant. The pre-operative periapical radiograph revealed issues with both the left central and lateral incisor teeth [FIGURE 1]. The pre-operative CBCT was accomplished with the “lift-lip” cotton-roll technique to separate the lip from the alveolus (cyan arrows) to better assess the buccal plate and extent of the vestibule [FIGURE 2a]. A facial concavity was evident beyond the apex of the root, limiting the buccal-palatal width of available bone for implant placement.
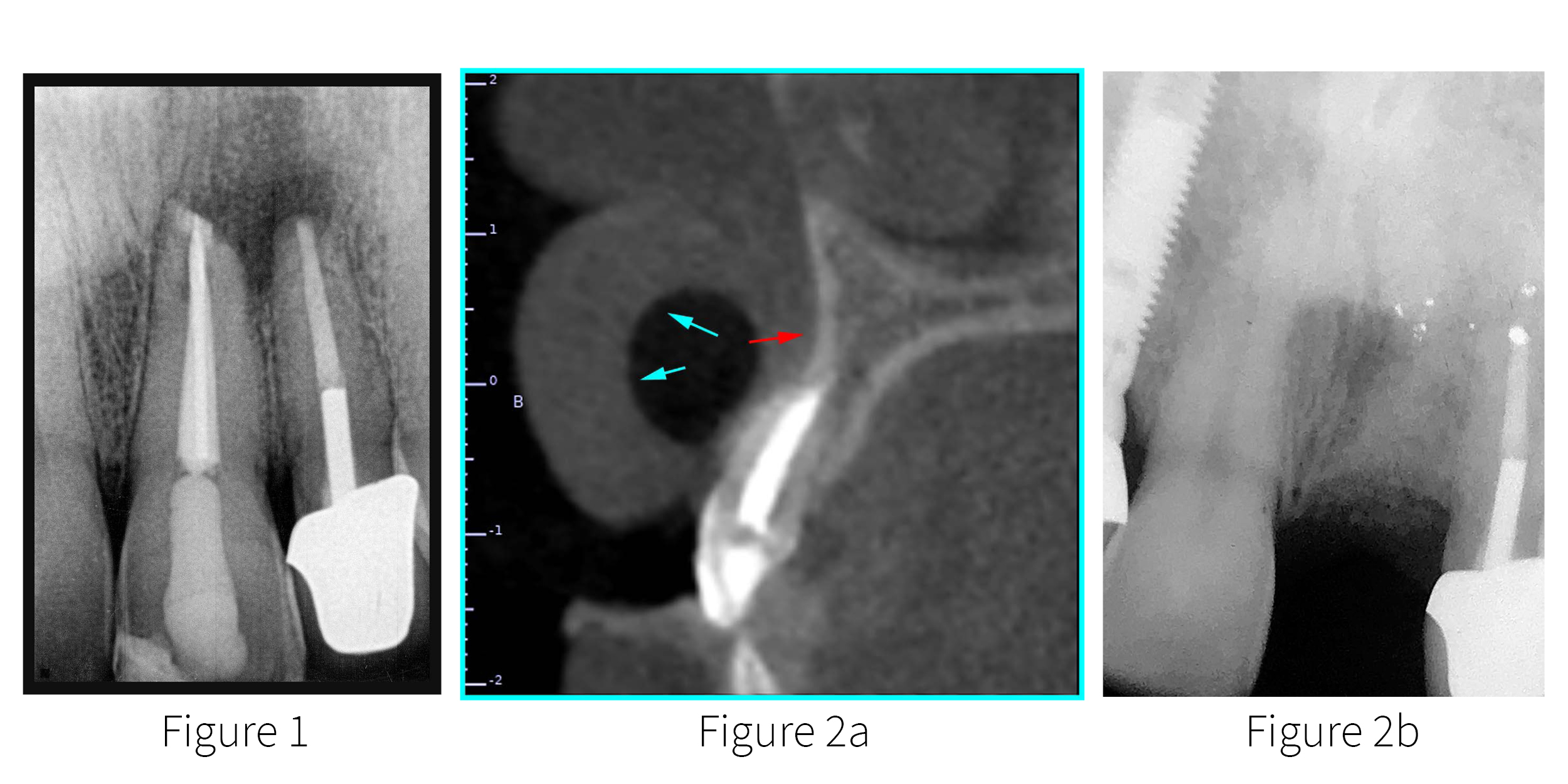
Figure 1. Pre-op periapical radiograph revealing failing central incisor tooth
Figure 2a. Pre-op CBCT illustrating the “lip-lift” technique (cyan arrows) to lift the lip off
of the alveolar bone. The red arrow points to the concavity above the apex of the root.
Figure 2b. Post-grafting periapical radiograph.
Upon careful extraction and proper debridement, socket preservation and augmentation with corticocancellous bone was completed, along with an apicoectomy for the lateral incisor tooth. The area was allowed to heal for five months during which time the patient wore a removable partial denture. A two-dimensional periapical radiograph revealed the grafted site at five months [FIGURE 2b].
Using a papilla-sparing flap design, a soft-bone drilling protocol was utilized to engage grafted bone in the maxillary receptor site using “template-assisted” guidance (not shown). A 3.5 mm diameter by 13 mm length implant was placed (AnyRidge, Integrated Dental Systems (IDS) – MegaGen, Englewood, NJ). As this was grafted bone it was important to have an objective baseline of implant stability. The initial Osstell implant stability quotient (ISQ) was 68 [FIGURE 3]. It was elected not to immediately load the implant, and the soft tissue was approximated and sutured to achieve primary closure. The favorable design of the implant, combined with the initial Osstell ISQ value provided a high level of confidence to determine that an accelerated eight week healing period would be sufficient to achieve the integration necessary for restorative loading.
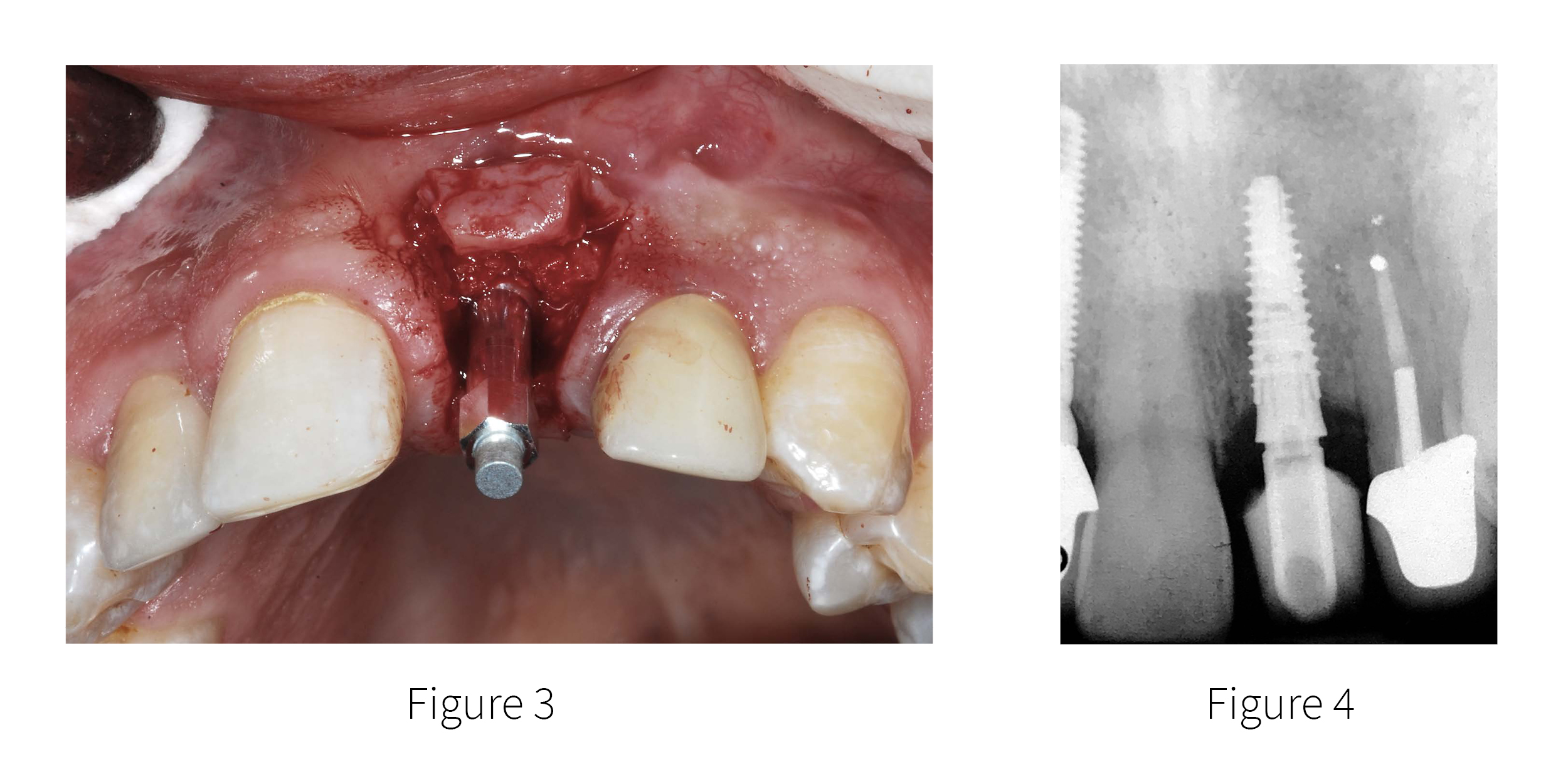
Figure 3. The SmartPeg ready for Osstell ISQ measurement after implant placement.
Figure 4. A screw-retained temporary was fabricated to aid in the maturation of the soft
Tissue sulcus.
At approximately 8 weeks the patient returned to uncover the implant. To assess the level of osseointegration, secondary Osstell ISQ values were recorded at 76 buccal, and 76 palatally, indicating improved stability. The increase in Osstell ISQ provided the confidence for restorative loading with a transitional screw-retained restoration fabricated to also assist in soft tissue maturation and emergence profile [FIGURE 4]. Therefore resonance frequency analysis (RFA) provides the practitioner with an accurate and objective measure of the osseointegration process and subsequent changes over time.
Once the soft tissue sulcus had matured, a fixture level impression recorded the position of the implant so that the definitive restoration could be completed by the dental laboratory. The morphology of the screw-retained restoration mimicked the natural emergence profile of the natural tooth as illustrated mounted on the blue analog [FIGURES 5a-c].
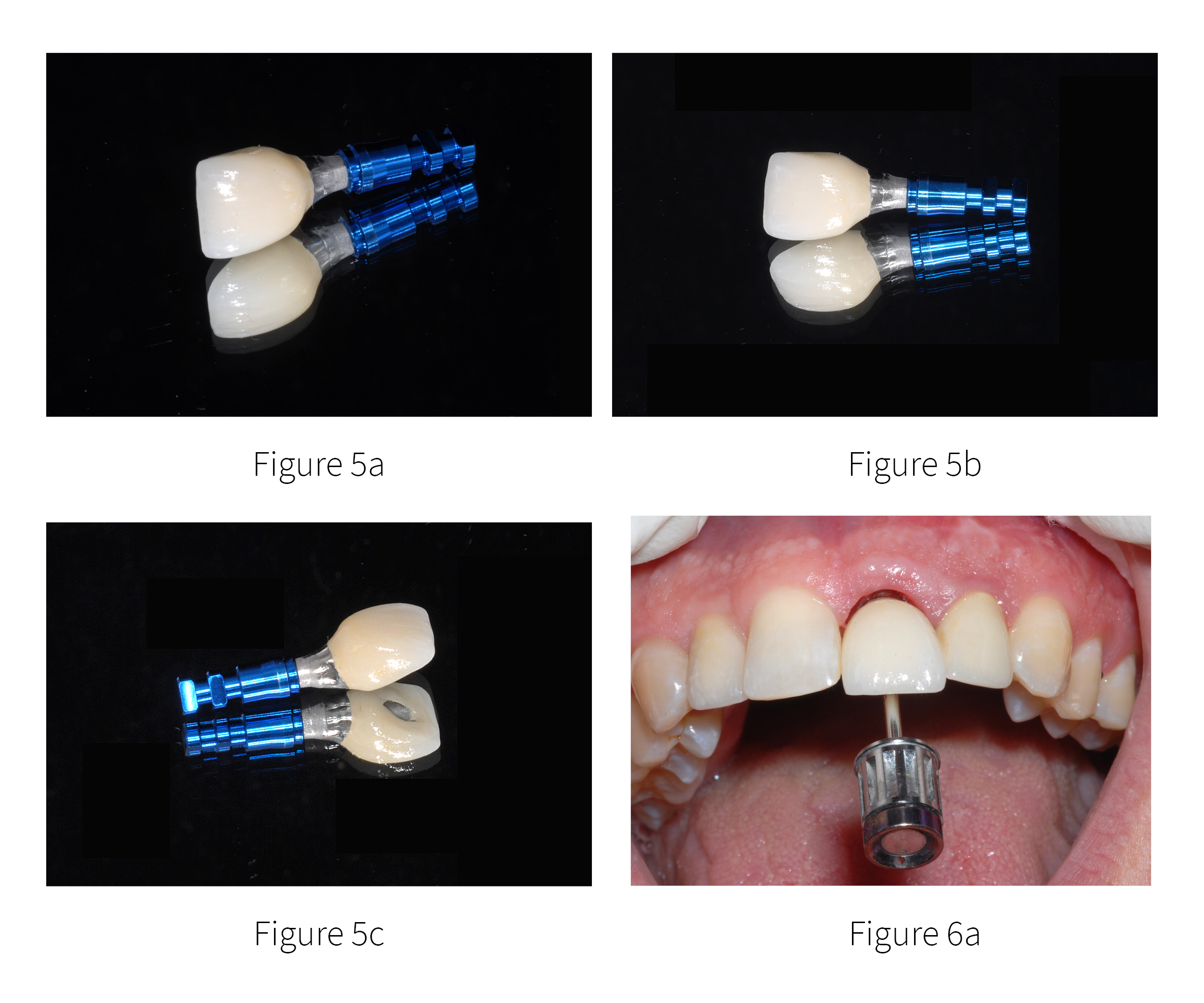
Figure 5a,b,c. The screw-retained restoration mimicked the natural emergence profile of the natural tooth as illustrated mounted on the blue analog.
The maintenance of the interdental papilla was achieved through development of the emergence profile using first the temporary restoration, followed by the definitive prosthetic crown screw-retained direct to the implant [FIGURES 6a & 6b]. The final periapical radiograph is seen in FIGURE 7. Note the similarities between shape of the natural right central incisor root and the tapered design of the AnyRidge implant, and the adjacent pre-existing implant for the right lateral incisor placed 14 years prior.
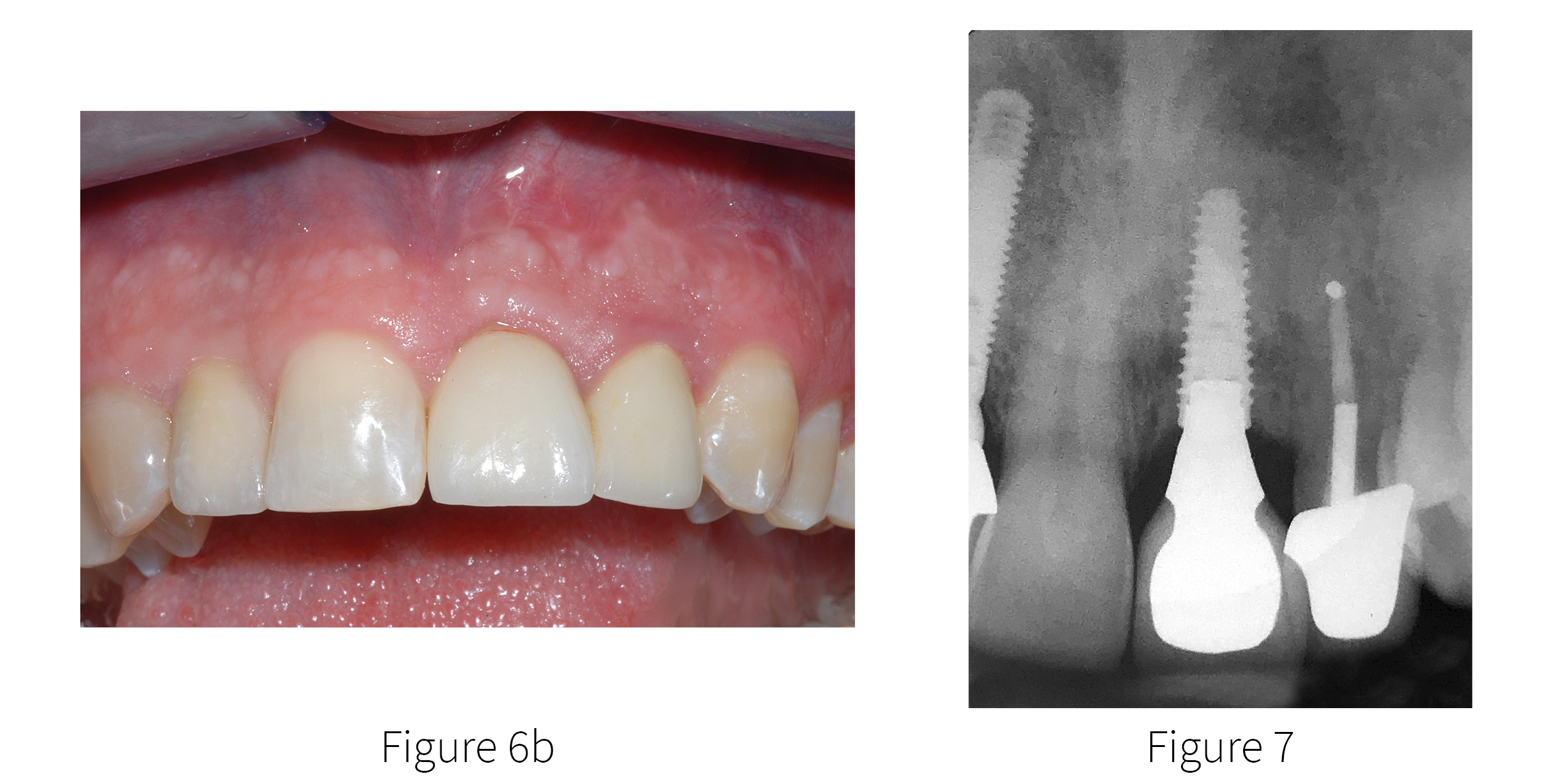
Figure 6a,b. The final screw-retained crown, illustrating excellent maintenance of the interdental papilla and emergence profile.
Figure 7. The final periapical radiograph reveals the interproximal levels of bone and
contours of the abutment seated on the well-integrated implant.
The placement and restoration of dental implants requires an appreciation of the patient’s unique anatomy whether for a single tooth or full arch restoration. The use of CBCT imaging and interactive software provide clinicians with the tools to assess the pre-existing clinical presentation, bone density, thickness and opacity of cortical plates, width of available bone, adjacent vital structures, and any pathology that may be involved. However, accurate planning even coupled with guided surgical protocols cannot definitively determine implant stability. This brief case review involved a failing maxillary central incisor which did not have enough bone volume to place an immediate implant after extraction. Bone grafting was necessary to gain the lost bony architecture for subsequent successful implant reconstruction.
Whether an implant is to be placed in a healed site, an immediate extraction site, or a grafted site, stability of the implant(s) is essential for successful osseointegration and ultimate restoration. It is important to note that stability can, and should be measured at different times; at initial placement, at uncovering in a delayed approach, to determine when an implant can be loaded, and throughout the lifespan of the implant if possible. It has been well documented that Resonance Frequency Analysis (RFA) provides a true objective assessment regarding implant stability providing clinicians with a necessary surgical and restorative tool to determine status of integration, and when an implant can be restored. The current case presentation noted Osstell ISQ values at placement and then when the implant was uncovered using the non-destructive technology of resonance frequency analysis. A screw-retained single tooth replacement as demonstrated helped in the modification of the surrounding soft tissue sulcus, while allowing for a level of retrievability if future assessment of implant stability will be desired. The positive increase of Osstell ISQ values became a medical-legal notation in the patient record, and contributed to a high level of confidence to proceed to the final restorative result.


Add comment